What is Ventricular Tachycardia?
The ventricles are the heart's two lower chambers. They fill with blood from the top chambers of the heart (atria) and send it to the lungs and through the aorta to be circulated throughout the body. Tachycardia is a heart rate of greater than 100 beats per minute. A normal heart rate is 60 to 100 beats per minute at rest. Ventricular tachycardia is a regular, faster-than-normal heart rate that begins in the heart's lower chambers. In most patients with ventricular tachycardia, the rate is in the range of 170 beats per minute or more.
What causes Ventricular Tachycardia?

Normal heartbeats from 60-100 times a minute when resting. These heartbeats originate in the right upper chamber (there are two upper chambers, the atria, and two lower chambers, the ventricles, in the heart), called the right atrium, with an electrical impulse produced by a natural pacemaker called the sinus node. The sinus node produces an electrical impulse that starts a normal heartbeat.
These impulses travel across both atria, causing the atria muscles to contract and pump blood into the ventricles, the lower chambers.
The electrical impulses arrive at a cluster of cells called the atrioventricular node, the pathway for signals to cross from the atria to the ventricles. This node creates a slight delay before sending the impulse to the ventricles. This allows the ventricles to fill with blood. Then the ventricles receive the impulse and they contract, pumping the blood to the lungs or the rest of the body.
When a person has ventricular tachycardia, abnormal electrical signals occur in the ventricles causing the heart to beat faster than normal, usually over 100 beats a minute, and this is out of sync with the atria. Now the heart may not be able to pump enough blood to your body and lungs because the chambers are beating so fast or are so out of sync that they don’t have time to fill properly before pumping.
Symptoms of V-Tach
During an episode of ventricular tachycardia, the heart is beating so fast that the blood pressure drops so the heart cannot pump enough oxygen to every part of the body, and this is what causes symptoms. Although some people with ventricular tachycardia do not experience any symptoms, the most common symptoms are:
- Dizziness
- Lightheadedness
- Palpitations
- Shortness of breath
- Chest pain
When the heart rate is extremely high or the ventricular tachycardia persists for more than a few seconds, it can cause fainting, unconsciousness or cardiac arrest and death.
What our patients have to say
"I became a patient of Dr. Smith in an emergency situation. Had that not been the case and I had time to choose, I would NOT CHANGE A THING! I am so very thankful."
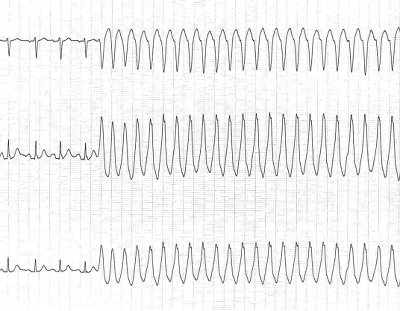
How is Ventricular Tachycardia diagnosed?
Dr. Smith will start by reviewing your symptoms and your family and personal medical history. He will then conduct a physical examination. If not deemed a medical emergency he may require a variety of possible tests to diagnose your ventricular tachycardia. These include an electrocardiogram, cardiac imaging, stress test, and electrophysiological test.
Electrocardiogram
The most common tool to diagnose ventricular tachycardia is an electrocardiogram (ECG). An ECG detects and records your heart’s electrical activity using electrodes attached to your chest and arms. An ECG records the timing and strength of electrical signals as they travel through your heart. Dr. Smith can look for patterns with these signals to determine what kind of tachycardia you have.
He may also have you use portable ECG devices at home. These include:
- Holter monitor — This portable ECG device is carried in your pocket or worn on a belt or shoulder strap. It is wired to electrodes that are placed on your chest. The device monitors your heart’s activity for a 24-72 hour period. You’ll also keep a diary during the same period.
- Event monitor — Event monitors record your heart’s activity over a period of a few weeks to a few months. You wear the monitor all day, but it only records at certain times for a few minutes at a time. In most cases, you activate the monitor by pushing a button when you experience symptoms of a fast heart rate.
- Transtelephonic monitor — This device must be worn continuously. It provides continuous heart rhythm monitoring.
- Implantable loop recorder — This device can be placed under your skin for up to three years for continuous heart rhythm monitoring.
Cardiac Imaging
Dr. Smith may request imaging of your heart to look for structural abnormalities that may be contributing to your ventricular tachycardia. These are the types of cardiac imaging:
- Echocardiogram — Sound waves are used to create a moving picture of your heart.
- Magnetic resonance imaging — A cardiac MRI provides still or moving pictures of how the blood is flowing through the heart. It detects irregularities.
- Computerized tomography — A CT scan combines several X-ray images to provide a more detailed cross-section view of your heart.
- Coronary angiogram — Dye and special X-rays are used to study the flow of blood through your heart and blood vessels.
- Chest X-ray — X-rays can be used to create still images of your heart, showing if the heart is enlarged.
Stress Test
This test determines how your heart functions while it is working hard during the exercise when given medicine to speed your heart rate. Typically, electrodes are placed on your chest and you walk or run on a treadmill. Your heart function is monitored while you do this.
Electrophysiological Test
A catheter tipped with electrodes is inserted into an artery at your groin or neck and is guided up to the various spots in the heart, seeking to pinpoint the location of the problems with the heart’s circuitry.
V-Tach Treatment
The goal of treatment for Dr. Smith is to restore your normal heart rhythm, regulate your heart rate, and prevent future episodes. Treatment will depend if your ventricular tachycardia is nonsustained and resolves within 30 seconds, or if it is sustained and lasts more than 30 seconds.
Sustained ventricular tachycardia usually requires urgent medical intervention. This may involve restoring the normal heart rate by delivering a jolt of electricity to the heart via defibrillation or cardioversion. An injection of an anti-arrhythmic medication, such as lidocaine, can also treat sustained ventricular tachycardia and restore a normal heart rhythm.
For patients with nonsustained or some cases of sustained ventricular tachycardia, the goal is to prevent future episodes and their possible complications. Treatments to prevent ventricular tachycardia include:
- Catheter ablation — A catheter with electrodes at the tip is inserted through the groin or neck artery and is guided to the heart. There, the electrodes use heat, extreme cold, or radiofrequency energy to damage/ablate the electrical pathway sending the incorrect electrical signals.
- Medications — Anti-arrhythmic medications can be taken regularly to prevent a fast heart rate.
- Implantable cardioverter-defibrillator — If you could have a life-threatening ventricular tachycardia event, Dr. Smith may recommend an implantable cardioverter-defibrillator. These are implanted in the chest and they continuously monitor your heartbeat. If an increase is detected, the device delivers calibrated electrical shocks, restoring normal rhythm.
- Surgery — Surgery is only used as a last resort when other treatment options are not working, or if surgery is needed to treat another heart disorder..
Ventricular Tachycardia vs. Atrial Tachycardia
Any tachycardia is defined as a heart rate of over 100 beats per minute. The difference between atrial tachycardia and ventricular tachycardia is the origination of the incorrect electrical impulses. In atrial tachycardia, the signals originate in the upper chambers, the atria, of the heart. In ventricular tachycardia, they originate in the lower chambers, the ventricles.
How can you prevent Ventricular Tachycardia?
The most effective way to prevent ventricular tachycardia is to reduce your risk of developing heart disease. To reduce this risk you should follow these steps: exercise, eat a healthy diet, maintain a healthy weight, keep your blood pressure and cholesterol levels under control, stop smoking, drink in moderation, don’t use recreational drugs, control your stress, and limit your caffeine intake.
Schedule a Consultation
If you are experiencing symptoms of Ventricular Tachycardia, call 205-971-7566 to schedule a consultation with Dr. Macy C. Smith.