It can be disconcerting when you feel a fluttering or skipped beat in your chest. You’ve just had a premature ventricular contraction (PVC). PVCs are actually extra heartbeats that begin in one of your heart’s two lower pumping chambers, the ventricles. These extra beats disrupt your heart’s normal rhythm and can create that feeling of missing a beat.
Premature ventricular contractions occur in many people, and if you’re otherwise healthy and occasionally have a PVC there isn’t anything to worry about. However, if these are a frequent occurrence, then a call to Dr. Smith, Birmingham’s heart rhythm specialist, is in order.

What are Premature Ventricular Contractions?
Premature ventricular contractions (PVCs) are extra, abnormal heartbeats that begin in one of your heart's two lower pumping chambers (ventricles). These extra beats disrupt your regular heart rhythm, sometimes causing you to feel a flip-flop or skipped beat in your chest.
What causes Premature Ventricular Contractions?
To understand what’s going on with PVCs, it helps to first know how the normal heart beats. Our hearts have two upper chambers, the atria, and two lower chambers, the ventricles. Our heart rhythm is controlled by the sinoatrial node (sinus node), an area of specialized cells in the right atrium. Electrical impulses originate in the sinus node and they travel across the atria to the ventricles, causing them to contract and pump blood out to the lungs and body.
When you have a PVC, these abnormal contractions usually occur in front of the next regular heartbeat. This disrupts the normal order of pumping: atria first, and then the ventricles.
Why this happens isn’t always easy to pinpoint. It’s thought that certain triggers, heart diseases, or changes in the body can make cells in the ventricles electrically unstable, allowing these extra heartbeats.
PVCs are also associated with:
- Increased levels of adrenaline in the body due to caffeine, tobacco, exercise, or anxiety
- Certain medications, including decongestants and antihistamines
- Alcohol or illegal drugs
- Injury to the heart muscle from coronary artery disease, congenital heart disease, high blood pressure, or heart failure
Symptoms of PVC’s
When a PVC occurs as a single premature beat, patients may describe the feeling as a "palpitation" or "skipped beat." The beat following the PVC can be strong enough to cause pain or discomfort in the chest. Individuals who have frequent PVCs or a series of them may experience a fluttering sensation in the chest or neck. If PVCs are frequent enough to reduce the heart's pumping ability, the individual may experience weakness, dizziness or fainting.
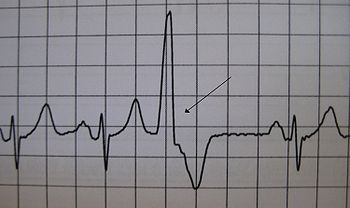
How does Dr. Smith diagnose a PVC?
Dr. Smith uses an electrocardiogram (ECG) for diagnosis. ECGs can detect the extra beats and identify the pattern and source. There are different options here, so he may use a standard ECG or other options.
Standard ECG: Electrical sensors are attached to the patient’s chest and limbs. These sensors will create a graphical record of the electrical signals traveling through your heart. Dr. Smith performs ECGs in his Birmingham offices.
If your PVCs are infrequent or irregular, they may not show up on a standard ECG. For these patients, Dr. Smith could use a portable ECG, such as a Holter monitor or an event recorder, or he may call for an exercise stress ECG.
Real Patient Testimonial About Dr. Macy Smith
"Definitely one of the best cardiologist in the country in all categories."
How are PVCs different than other Arrhythmias?
Arrhythmias are generally divided into two categories: ventricular and supraventricular. Ventricular arrhythmias occur in the lower chambers of the heart, the ventricles. Premature ventricular contractions are in this category. Supraventricular arrhythmias occur in the area above the ventricles, usually in the upper chambers of the heart, the atria. Irregular heartbeats can also be categorized as either too slow, bradycardia, or too fast, tachycardia.
For regular people, the most well known irregular heartbeat is atrial fibrillation. This is a fast, irregular rhythm where single muscle fibers in your heart twitch or contract. Atrial fibrillation is the main cause of stroke.
How are PVCs treated?
In people with healthy hearts, occasional PVCs are harmless, and they usually resolve on their own without treatment. Some PVC triggers, such as limiting caffeine, tobacco, or stress, can be managed to limit the occurrence.
However, if you experience PVCs regularly, this needs to be treated. This is particularly true if you have heart disease.
- Medications: Beta blockers, which are often used to treat high blood pressure and heart disease, can suppress PVCs. If you have ventricular tachycardia or frequent PVCs, other medications such as calcium channel blockers or anti-arrhythmic drugs can be helpful.
- Radiofrequency Catheter Ablation: If medications and changes in lifestyle don’t effectively manage your PVCs, Dr. Smith may recommend catheter ablation. During cardiac ablation, Dr. Smith uses radiofrequency energy to cauterize the area of the heart where the PVCs originate.
Can you prevent PVCs?
Prevention is possible, especially if you suffer from infrequent PVCs. Generally these are simply lifestyle changes. This would involve eliminating or curtailing intake of caffeine, alcohol, tobacco, and various illegal drugs such as cocaine. Also, lowering your high blood pressure or managing your stress and anxiety can prevent future PVCs.
Are there certain risk factors involved with PVCs?
All of these items or conditions can increase a person’s risk of having a PVC:
- Exercise
- Caffeine, tobacco, alcohol, illegal drugs
- High blood pressure
- Anxiety
- Various heart diseases
Schedule a Consultation
If you experience symptoms of Premature Ventricular Contractions, call 205-971-7566 today! Macy C. Smith, Jr., MD, FACC, FHRS serves Birmingham, Alabama and surrounding areas.